Understanding Ageing & Dullness


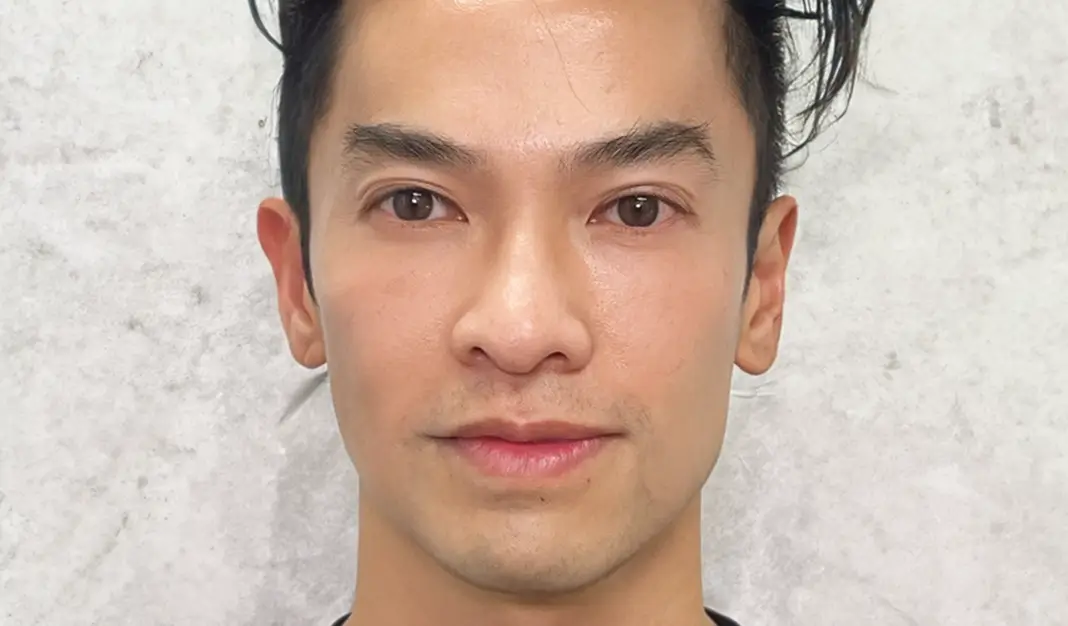
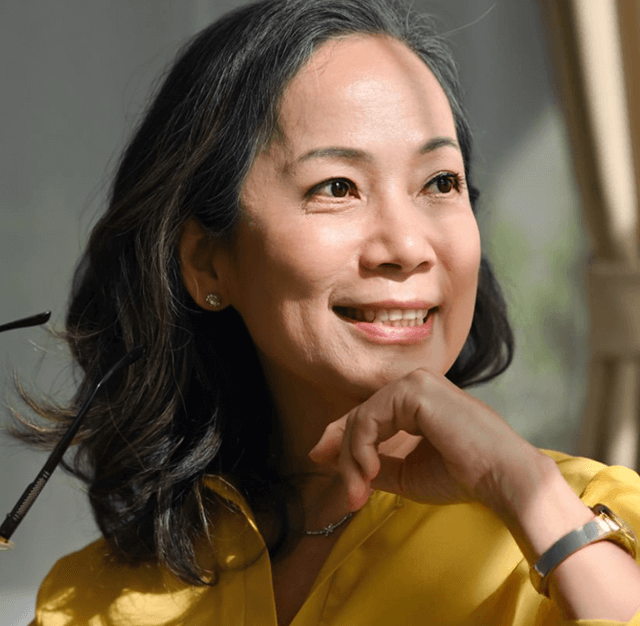
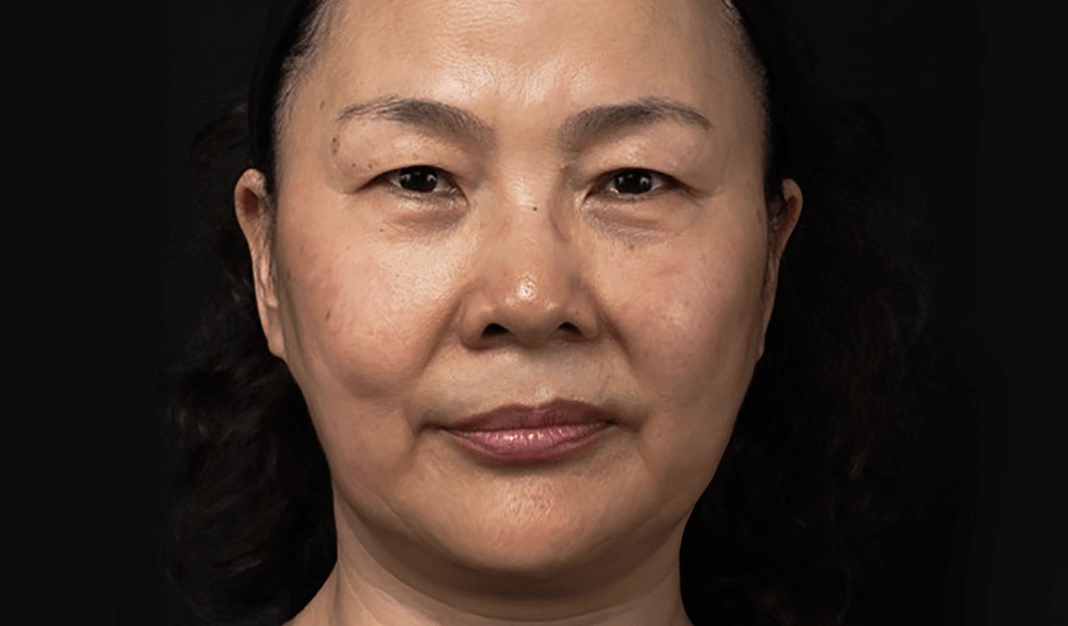
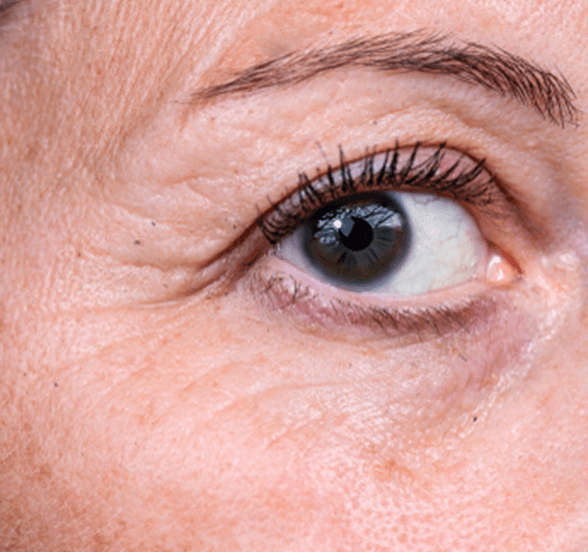
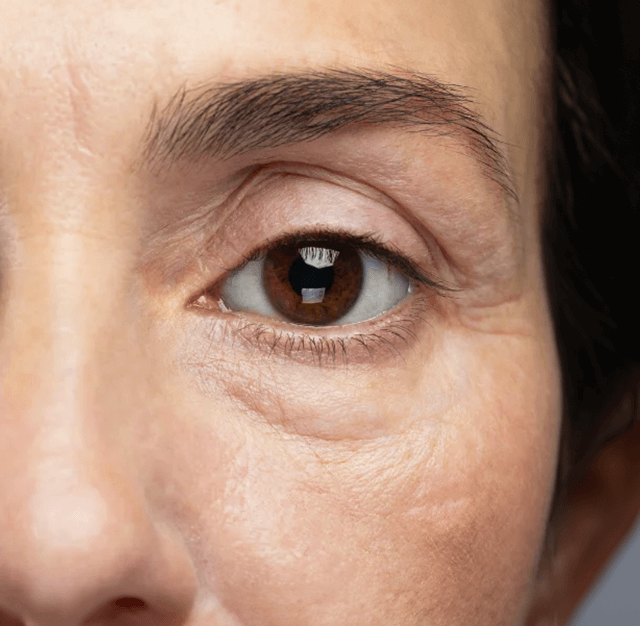
Conditions Across Life Stages








Common Conditions










We're here to help you manage your skin concerns.
At Folke®, we offer treatments and skincare products designed to support skin health, with results varying based on factors like skin type, conditions, lifestyle, and treatment adherence. Our information is based on in-clinic observations, client experiences, and published academic materials. While claims and comparisons to mainstream therapies reflect general research, reactions to treatments can vary. Not every patient will experience the same results, and some may tolerate treatments better than others. Folke®, its founder Charles Ng, staff, and representatives are not responsible for discrepancies or differing opinions. This content is for educational purposes and should not replace professional medical advice, diagnosis, or treatment. While Folke® is committed to high-quality treatments and products for skin concerns, individual outcomes may vary. The effectiveness of our treatments depends on various factors, and Folke® cannot guarantee specific results for every client. We encourage clients to consult with our professionals to set realistic expectations tailored to their needs. This information should not replace professional medical advice or treatment.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Sadick NS et al., “The impact of collagen production on skin ageing.” Journal of Clinical and Aesthetic Dermatology 13, no. 6 (2020): 18-25.
Sivamani RK et al., “Natural alternatives for treating aging skin and inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Passeron T et al., “Melasma and aging: Pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and aging treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Alvarez OM et al., “Botanical extracts for skin lightening and anti-aging: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Boonchai W et al., “Post-inflammatory hyperpigmentation and aging: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Grimes PE et al., “Histologic changes in hyperpigmented skin.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Nistico SP et al., “Efficacy of botanical formulations for managing aging and hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Draelos ZD et al., “Efficacy of natural ingredients in anti-aging and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Redefining Ageing, Naturally
Plant-Based, Non-Invasive Approach


Outside-In, Inside-Out Approach




Beyond Quick Fixes




Avoid Depletion of the Fat Layer


Cumulative Collagen Farming

Reduce the Onset of Static Wrinkles


Personalised and Sustainable Solutions

We're here to help you manage your skin concerns.
At Folke®, we offer treatments and skincare products designed to support skin health, with results varying based on factors like skin type, conditions, lifestyle, and treatment adherence. Our information is based on in-clinic observations, client experiences, and published academic materials. While claims and comparisons to mainstream therapies reflect general research, reactions to treatments can vary. Not every patient will experience the same results, and some may tolerate treatments better than others. Folke®, its founder Charles Ng, staff, and representatives are not responsible for discrepancies or differing opinions. This content is for educational purposes and should not replace professional medical advice, diagnosis, or treatment. While Folke® is committed to high-quality treatments and products for skin concerns, individual outcomes may vary. The effectiveness of our treatments depends on various factors, and Folke® cannot guarantee specific results for every client. We encourage clients to consult with our professionals to set realistic expectations tailored to their needs. This information should not replace professional medical advice or treatment.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Hassim Z et al., “Hormonal influences on aging and hyperpigmentation: A comprehensive review.” International Journal of Women’s Dermatology 6, no. 2 (2020): 73-82.
Briganti S et al., “Melanin: What is it and how is it produced?” International Journal of Cosmetic Science 25, no. 6 (2003): 279-289.
Solano F, “Melanins: Skin pigments and much more—types, structural models, biological functions, and formation routes.” New Journal of Science 2014 (2014): 1-28.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Draelos ZD et al., “Efficacy of natural ingredients in anti-aging and skin lightening.” Journal of Drugs in Dermatology 18, no. 6 (2019): 586-591.
Alvarez OM et al., “Botanical extracts for skin lightening and anti-aging: Efficacy and safety.” Journal of Cosmetic Dermatology 17, no. 6 (2018): 1067-1074.
Nistico SP et al., “Efficacy of botanical formulations for managing aging and hyperpigmentation.” Journal of Dermatological Treatment 31, no. 4 (2020): 395-402.
Sivamani RK et al., “Natural alternatives for treating aging skin and inflammation.” Journal of Drugs in Dermatology 18, no. 8 (2019): 788-794.
Passeron T et al., “Melasma and aging: Pathogenesis and treatments.” Dermatologic Clinics 32, no. 3 (2014): 291-299.
Katsambas A et al., “Hyperpigmentation and aging treatment strategies.” Journal of the European Academy of Dermatology and Venereology 23, no. 7 (2009): 751-760.
Boonchai W et al., “Post-inflammatory hyperpigmentation and aging: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Poon TS et al., “Age-related changes in hyperpigmentation and effective management strategies.” Journal of Clinical and Aesthetic Dermatology 14, no. 7 (2021): 32-40.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Considerations with Mainstream Treatments
Cosmetic Procedures
01 • Less Long-Term Results




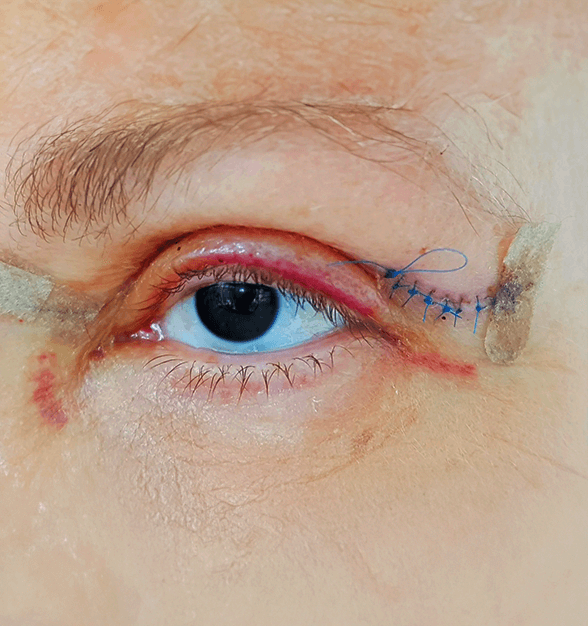
02 Increased Sensitivity and Downtime


03 Risk of Collagen and Fat Layer Depletion


04 Unnatural Appearance

05 • Scarring and Prolonged Recovery in Surgical Options



Topical Treatments
01 Limited Penetration and Superficial Impact



02 Potential for Long-Term Irritation


03 • Heightened Photosensitivity
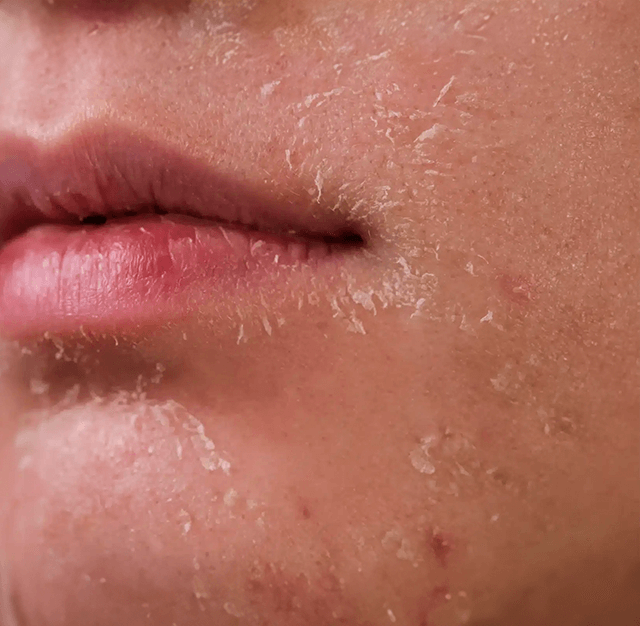

04 Minimal Effect on Structural Concerns

We're here to help you manage your skin concerns.
Sadick NS et al., “Volume loss and filler fatigue: Understanding the longevity of injectable fillers.” Dermatologic Surgery 43, no. 6 (2017): 848-855.
Goldberg DJ et al., “Pigment-safe laser treatments for aging skin.” Journal of Cosmetic and Laser Therapy 17, no. 6 (2015): 314-320.
Chung JH et al., “Long-term outcomes of CO2 laser treatment for pigmentation.” Journal of Dermatological Treatment 29, no. 4 (2018): 365-370.
Dika E et al., “Laser treatment for benign melanocytic nevi: A review.” Lasers in Medical Science 33, no. 4 (2018): 853-861.
Narins RS et al., “Safety of hyaluronic acid fillers: A comprehensive review.” Dermatologic Surgery 37, no. 10 (2011): 1697-1705.
Matarasso SL et al., “Complications of soft tissue augmentation: Prevention and management.” Journal of the American Academy of Dermatology 66, no. 1 (2012): 11-22.
Al-Niaimi F et al., “Managing hyperpigmentation post-laser therapy.” Journal of Cosmetic and Laser Therapy 20, no. 3 (2018): 157-163.
Fabi SG et al., “Collagen stimulation and neoformation: A review of the science behind dermal fillers.” Journal of Drugs in Dermatology 13, no. 9 (2014): 1044-1052.
Grimes PE et al., “Histologic changes in aging skin and its management.” Journal of the American Academy of Dermatology 55, no. 5 (2006): 768-775.
Boonchai W et al., “Post-inflammatory hyperpigmentation: Risk factors and prevention.” International Journal of Dermatology 55, no. 5 (2016): 487-495.
Lim JT et al., “Sun protection and prevention of aging and hyperpigmentation.” Journal of the American Academy of Dermatology 82, no. 5 (2020): 1236-1245.
Bolognia JL et al., “Complications of lasers and light-based devices in dermatology.” Dermatologic Therapy 26, no. 5 (2013): 332-343.
Rodriguez CI et al., “Role of oxidative stress in aging and hyperpigmentation: Mechanisms and treatments.” Journal of Clinical and Aesthetic Dermatology 12, no. 4 (2019): 28-35.
Del Rosario C et al., “Tyrosinase inhibitors: Strategies to control melanin production in aging and hyperpigmentation disorders.” International Journal of Molecular Sciences 22, no. 11 (2021): 6150.
Baumann L et al., “Chemical peels: An evidence-based review.” American Journal of Clinical Dermatology 10, no. 6 (2009): 297-306.
Aldahan AS et al., “Topical treatments for melasma, aging, and hyperpigmentation.” Journal of Clinical and Aesthetic Dermatology 11, no. 2 (2018): 19-23.
Kraft JN et al., “The role of inflammation in aging and hyperpigmentation management.” Journal of Clinical and Aesthetic Dermatology 11, no. 8 (2018): 16-23.
Grimes PE et al., “Management of exogenous ochronosis caused by topical hydroquinone in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Sardana K et al., “Rebound pigmentation and its management in aging and hyperpigmentation disorders.” Indian Journal of Dermatology, Venereology, and Leprology 85, no. 3 (2019): 243-250.
Handog EB et al., “Challenges in the management of hyperpigmentation and aging: Prevention and treatment.” Journal of Clinical and Aesthetic Dermatology 9, no. 1 (2016): 15-24.
Bikowski JB et al., “Prevention and management of post-inflammatory hyperpigmentation in aging skin.” Journal of Drugs in Dermatology 17, no. 9 (2018): 925-932.
Verallo-Rowell VM et al., “Safety and efficacy of botanical agents in managing aging and hyperpigmentation.” Dermatologic Therapy 33, no. 5 (2020): e13963.
Hassim Z et al., “Management of collagen depletion and fat layer loss in aging skin.” Journal of Dermatology 47, no. 5 (2020): 431-437.
Narins RS et al., “Long-term complications of injectable soft tissue fillers: A review.” Dermatologic Surgery 34, no. 12 (2008): 1574-1579.